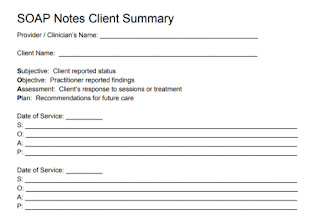
SOAP Notes
SOAP notes, AKA Subjective Objective Assessment Plan notes, are live-transcribed doctor-patient consultation-time conversations. As a medical scribe, you are supposed to do this the whole day. These are perfectly transcribed doctor-patient consultation-time conversations for you to read and upskill yourself.
2.


Comments
Post a Comment